20 year old male with fever and vomitings
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss out individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omit
chief complaints
A 20 year old male native of miryalguda came to OPD with a chief complaint of fever associated with vomitings since 9 days
History of present illness
patient was apparently asymptomatic 9 days back then he developed vomitings which were non projectile, watery, associated with nausea. There was no retching when he was outside and when he reached home had 2 episodes of vomiting 5 minutes apart which were non projectile, watery and associated with blood clots. Then he went to the local hospital and was given a medication (Zofer) and was suggested to get an endoscopy, Then he developed fever which was continuous high grade not associated with chills, rigor, rash and no diurnal variation
His daily life activity included consumption of outside food almost 5 times in the past week and on the next day endoscopy showed pan gastritis, fever continued throughout the day, the next day (Nov 30) he got admitted to the local hospital and was conservatively managed, he had continuous fever not associated with vomitings
on the next day he had 3 episodes of vomiting non projectile and watery, as the severity was increasing he was shifted to a higher center of health
On Sunday he had 8 episodes of vomitings starting at 3:30 am the vomitings were non projectile, watery immediately after consuming food associated with fever spikes then developed head ache and body pains
No history of burning micturition.
No history of cough or cold.
No history of neck stiffness.
No history of pain abdomen, loose stools.
No h/o NSAIDS intake
PAST HISTORY
No similar complaints in the past.
No history of diabetes, hypertension, asthma, tuberculosis, epilepsy.
Personal history
For the past one year he has been staying home after completing his ITA training
His daily routine includes waking up at 8:00 am occasionally breakfast then roams around with friends skipping lunch quite often roams around the locality with friends and reaches home by 10:00pm and has his dinner by 11:00pm
General examination
patient is conscious, coherent and cooperative , well oriented with time, place and person
He is moderately built and nourished
He has no pallor , icterus , cyanosis, clubbing ,generalized lymphadenopathy, edema.
vitals :
temperature:
BP : 110/70 mmhg
PR :101 bpm
RR: 16cpm
Systemic examination
Abdominal examination
INSPECTION
- Shape - Scaphoid, with no distention.
- Umbilicus - Inverted
- Equal symmetrical movements in all the quadrants with respiration.
- No visible pulsation, peristalsis, dilated veins and localized swellings.
PALPATION
- Local rise of temperature present.
- Mild enlargement of liver,
regular smooth surface , rounded
edges , non tender, moving with
respiration non pulsatile
- SPLEEN palpable just below the costal margin, smooth, rounded margins, non tender.
PERCUSSION
- Hepatomegaly : liver span of 14 cms with 2 cms extending
below the costal margin
- Fluid thrill and shifting dullness absent
AUSCULTATION
- Bowel sounds not heard.
-No bruit or venous hum.
CNS
Higher mental functions intact.
No signs of meningeal irritation.
Normal sensory examination
Normal motor examination.
Cerebellar signs are absent.
CVS
S1 S2 heard, no murmurs.
Respiratory system
Bilateral air entry present, Normal vesicular breath sounds on both sides.
Provisional diagnosis
fever under evaluation
pangastritis
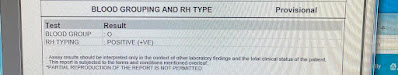
Investigations
Endoscopy ( outside the hospital )
On 3/12-
LFT
On 4/12
TREATMENT:
1. NBM
2. Inj.PAN 40mg in 100ml NS for 1 hr IV Stat
3. Inj.NEOMAL 1gm IV/SOS
4. Moniter vitals 4th hrly
5. Inform SOS
6. T.DOLO 650mg /po / tid
7. IVF @75ml/hr ( 2 ONS , 2ONL)
8. Inj.ZOFER 4mg IV/ TID
9. Inj. METROGYL 500mg IV/BD

























Comments
Post a Comment